As the EMS provider for more than 1 million people in the greater Fort Worth area, MedStar sees the use of the 9-1-1 system for medical and trauma conditions that, for the patient’s benefit, could best be addressed by a response other than an ambulance trip to an emergency department. In 2008, 21 individual patients were transported to area emergency rooms more than 2,000 times by MedStar, resulting in $962,429 in ambulance charges (not including the charges from the hospital emergency departments). Majority of these bills are uncollected. Many people are using EMS as a health care safety net.
In July 2009, MedStar implemented the Mobile Integrated Healthcare Program that identified high system users and developed individual care plans for each of those patients.
As part of that care plan, the enrolled patient receives regularly scheduled home visits by one of our Mobile Healthcare Providers. During those home visits, the paramedic provides a medical assessment, ensures the patient is taking their prescribed medications and is following up with their primary care provider. They also provide some often much-needed social interaction for these patients.
That humble beginning has led to the development and implementation of several programs all centered on Patient Navigation and Mobile Integrated Healthcare:
High Utilizer Group (“HUG”) Program
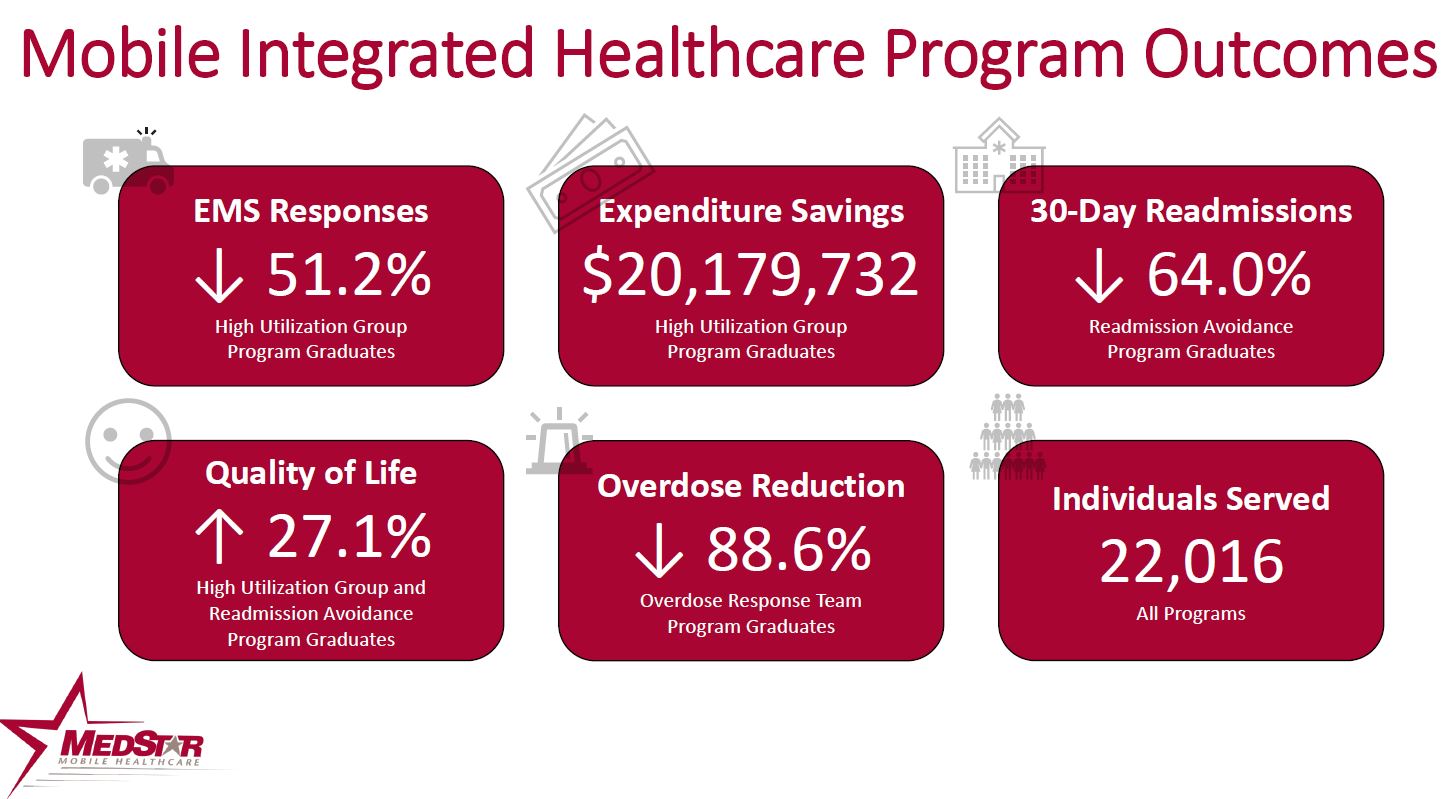
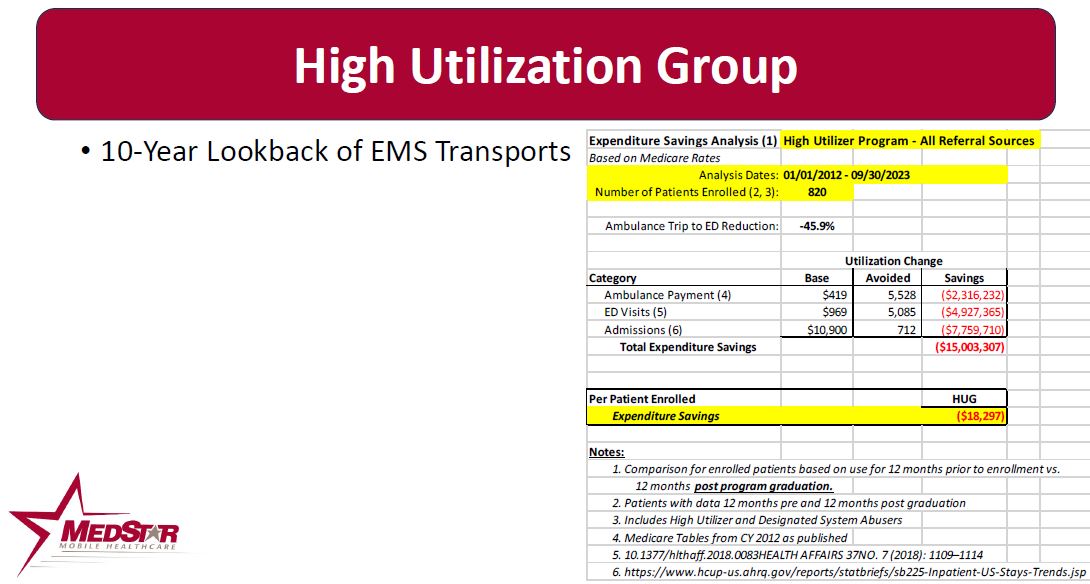
Patients who use 9-1-1 15 or more times in 90 days, or who are referred into the program by ED or payer case managers due to high ED utilization, are enrolled. MedStar’s Mobile Healthcare Providers (MHPs) conduct regular home visits, evaluate Social Determinants of Health, connect the patients to available resources and teach the patients how to better manage their own healthcare. Typical enrollment is 30-90 days. Since October 2013, 820 patients with 2 years of utilization data available (1 year pre and 1 year post enrollment) have reduced ambulance transports to the emergency department by 48.4% It also has prevented 5,545 ED visits in this patient population. This reduction has saved $15 million in healthcare expenditures for ambulance and ED admissions ($18,297 per enrolled patient).
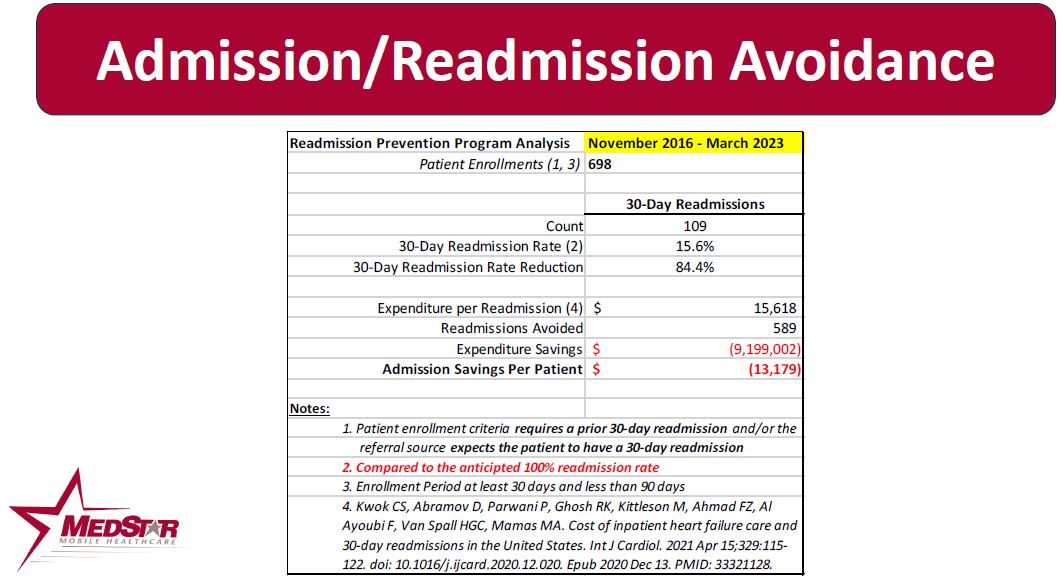
Readmission Avoidance
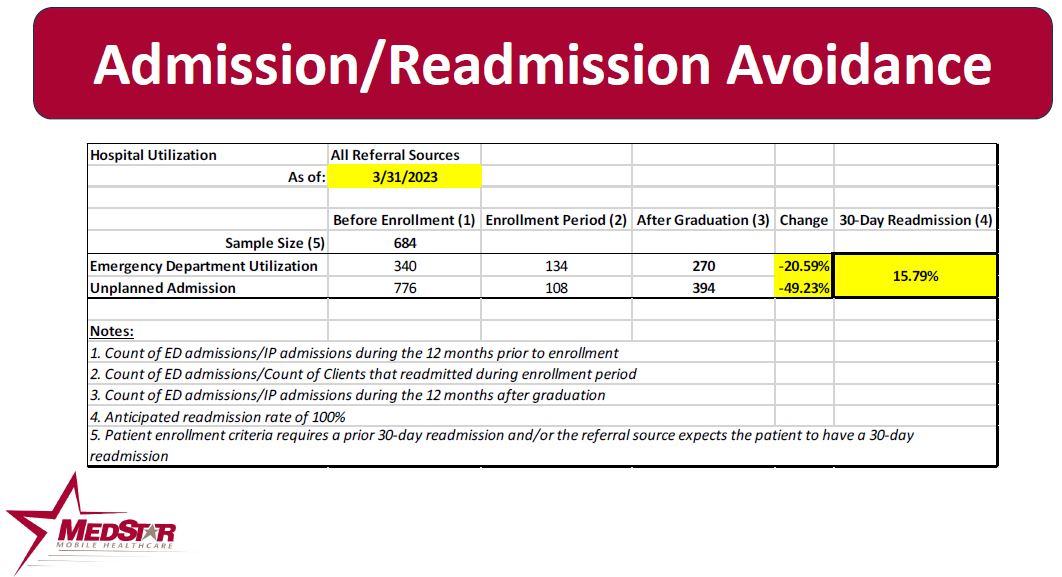
Patients at risk for a 30-day readmission are referred to MedStar by the patient’s Case Manager or PCP. MedStar conducts a series of home visits to educate the patient and family on appropriate care management and loops the patient to their PCP. If the patient needs intervention, the MedStar MHP may coordinate in-home diuresis or other treatments with the patient’s PCP, along with a follow-up PCP appointment. Since October 2013, 684 patients who had a prior 30-day readmission AND the referring agency felt would have a 30-day readmission have been referred into the program. The enrolled population had a 49.2% readmission rate versus the expected 100% readmission rate.
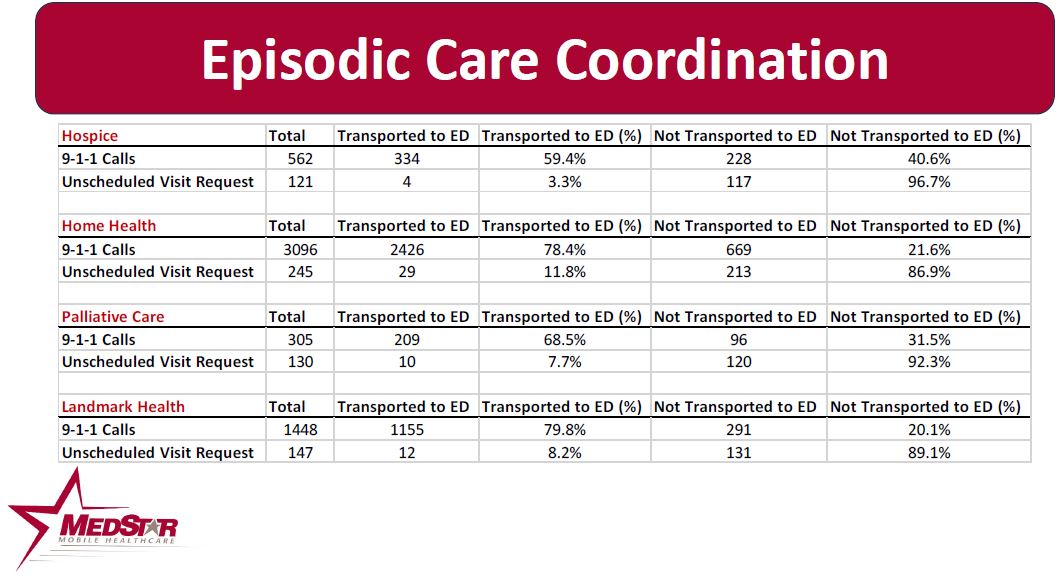
Episodic Care Coordination
MedStar works with numerous healthcare partners with special populations to help navigate patients to the most appropriate source of care for their medical needs. Sometimes this is during a 911 call, while at other times it’s a home visit requested by the partner agency. These partners include hospitals, health insurers, home health and hospice agencies, care management organizations, accountable care organizations and other partners. Through December 2023, of the 6,054 911 and urgent care responses to these enrolled patients, only 4,179 (69.0%) of the calls resulted in the patient being transported to an emergency department.
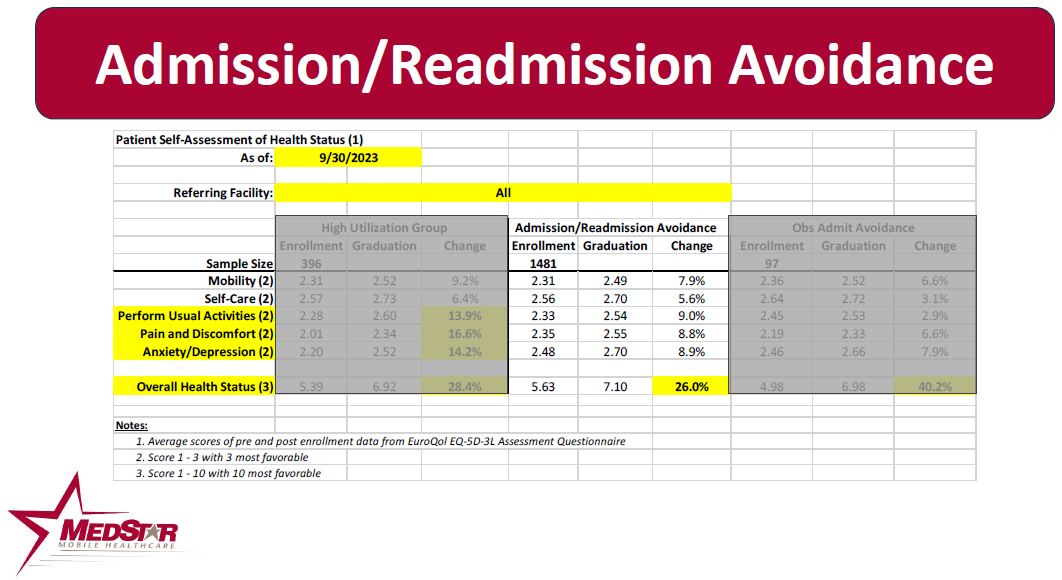
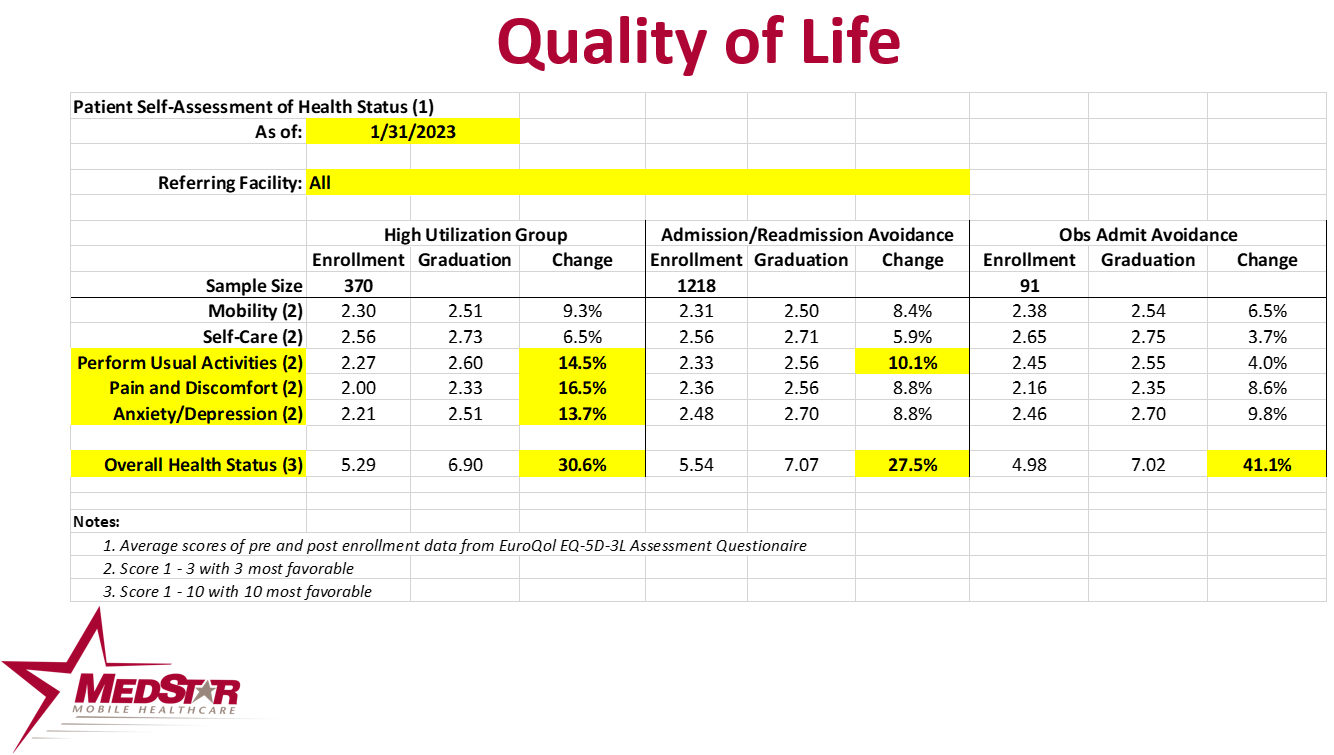
Patient Perception of Health Status
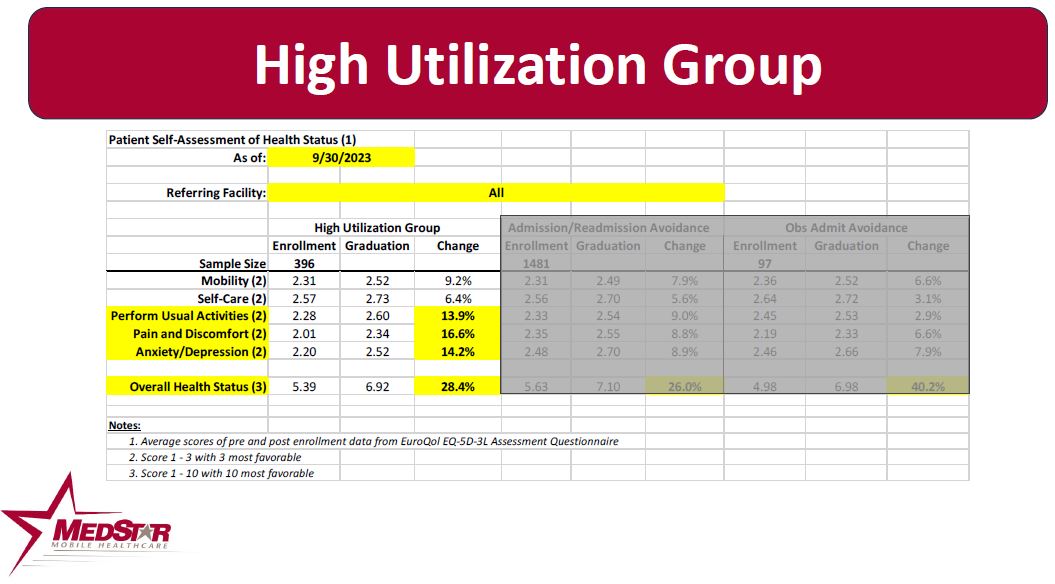
Patients enrolled in MedStar’s MIH programs are provided with a questionnaire to assess their perception of their health status upon enrollment in the program, and then upon graduation from the enrollment. These scores are then compared to assess how the patient’s perception of their health status has changed as a result of the enrollment. The chart below depicts the EuroQol score or the change in the patient’s perception of their health status.
The success of these programs would not be possible if it were not for our myriad of community partnership who have formed a unique collaborative to support enrolled patients with services and resources that contribute to their success!
The American Journal of Emergency Medicine published a study about MedStar’s MIH program.
Click here to review the peer-reviewed study.
The goal of the Mobile Healthcare Program is to meet the Institute for Healthcare Improvement’s Triple Aim:
– Improve patient outcomes, including their experience of care
– Improve the health of the population
– Reduce Costs
![]()
The Agency for Healthcare Research and Quality (AHRQ) has published MedStar’s MIH programs on the AHRQ Innovation Exchange in 2012, 2013, 2014, 2015 and 2016. Click Here to view the most recent AHRQ publication on the MIH programs.
For more information on how MedStar can assist you with the development and implementation of MHP programs in your local community, please submit a contact form and choose “Mobile Healthcare Program” as the “Topic” dropdown here
MedStar has hosted more than 226 communities from 46 states and 6 foreign nations for site visits to experience first-hand how these programs work. To request a site visit, please click on the link below.
MedStar Site Visit Request
The National Association of EMTs has taken the lead in promoting EMS-Based Mobile Integrated Healthcare programs to help EMS meet the Institute for Healthcare Improvement’s Triple Aim initiative.
Please view the video produced by NAEMT designed to educate EMS practitioners and other healthcare stakeholders on how EMS-Based MIH programs are transforming the EMS profession and achieving the Triple Aim!
View the Video Here
Jones and Bartlett Publishing has released a book written by MedStar’s Matt Zavadsky and Doug Hooten titled “Mobile Integrated Healthcare – Approach to Implementation”. This book walks you through the “why” and “how” of MIH programs.
Click here to be navigated to the Jones and Bartlett order site for MedStar’s MIH book.
Click on the links below to view some of the local media stories on these programs, the impact they have on our patients and the healthcare system.
CBS 11 Story on Status of MedStar MIH Programs
FOX 4 Story on the CHF Program
NEW REPORT:
Health Insight, the CMS Quality Improvement Network/Quality Improvement Organization for the State of Oregon published a comprehensive outcome report on the MIH programs in Oregon in June 2017.
Click here to view the report.
NEW VIDEO:
Quality Insights, CMS Quality Improvement Network/Quality Improvement Organization (QIN/QIO), recently published two EXCELLENT videos.
This one explains Community Paramedicine to patients:
https://www.youtube.com/watch?v=divguTHIszs
And, this one is an excellent Community Paramedicine overview for providers
https://www.youtube.com/watch?v=0BvU2kPr5Fk
Additional Mobile Healthcare Downloads & Reports:
- 2017 American Journal of Emergency Medicine Study of MedStar’s Readmission Prevention Program
- MedStar High Utilizer Program Overview
- MedStar High Utilizer Economic Report Through November 2021
- MedStar MIH Social Determinants of Health Report Through November 2021
- MedStar MIH Patient Experience Summary November 2021
- MedStar EuroQol MIH Program Health Status Scores Through November 2021
- MedStar Hospice Program Overview
- MedStar Hospice Revocation Avoidance Outcomes Through November 2021
- MedStar Home Health Partnership Overview
- Home Health / MedStar Partnership Report Through November 2021
- THR-HMFW Observation Admission Avoidance Program Outcomes Through November 2021
- MedStar Readmission Prevention Program Overview
- MedStar Readmission Prevention Program Outcomes Through November 2021 – THR-HMFW
- MedStar Readmission Prevention Program Outcomes Through November 2021 – THR-Alliance
- MedStar Readmission Prevention Poster
- Poster Presentation on DSRIP Medicaid Waiver Program
- 9-1-1 Nurse Triage Study Published March 2015 in Annals of Emergency Dispatch and Response
- 9-1-1 Nurse Triage Study Published February 2014 in Annals of Emergency Dispatch and Response
- MedStar Observation Admission Avoidance Program Overview
- 2016 University of Kansas Doctoral Thesis on MedStar’s Readmission Prevention Program
- University of California – San Francisco MIH-CP Research Report
- 2016 Agency for Healthcare Research and Quality Report on MedStar MIH Programs
Help Us Help the Community
 If you are a physician, hospital social worker or case manager you may refer someone into the Mobile Healthcare Program, click here to download a fillable or printable form.
If you are a physician, hospital social worker or case manager you may refer someone into the Mobile Healthcare Program, click here to download a fillable or printable form.
To refer a patient into our Hospice Revocation Avoidance program, click here to download a fillable or printable form.
Fax either, with supporting documentation, to: 817-632-0530.
To contact a representative of the MHP program for patient updates on admissions or discharges, call the MedStar communications center at 817-927-9620 and ask for the on-duty Mobile Healthcare Provider





