EMS providers have theorized that decreased 911 calls, and increased patient transport declination rates for patients experiencing cardiac-related symptoms may have led to increases in out-of-hospital-cardiac arrest (OHCA) cases and deaths.
A study just released in Health Affairs seems to support this theory.
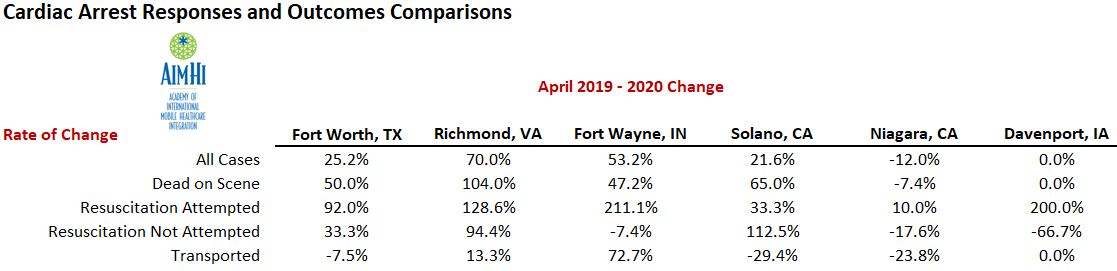
Previously released data from the Academy of International Mobile Healthcare Integration (AIMHI) revealed concerning trends reported by member agencies from:
- Fort Worth, TX: Metropolitan Area EMS Authority (MedStar)
- Richmond, VA: Richmond Ambulance Authority
- Fort Wayne, IN: Three Rivers Ambulance Authority
- Solano, CA: Medic Ambulance Service
- Davenport, IA: Medic EMS
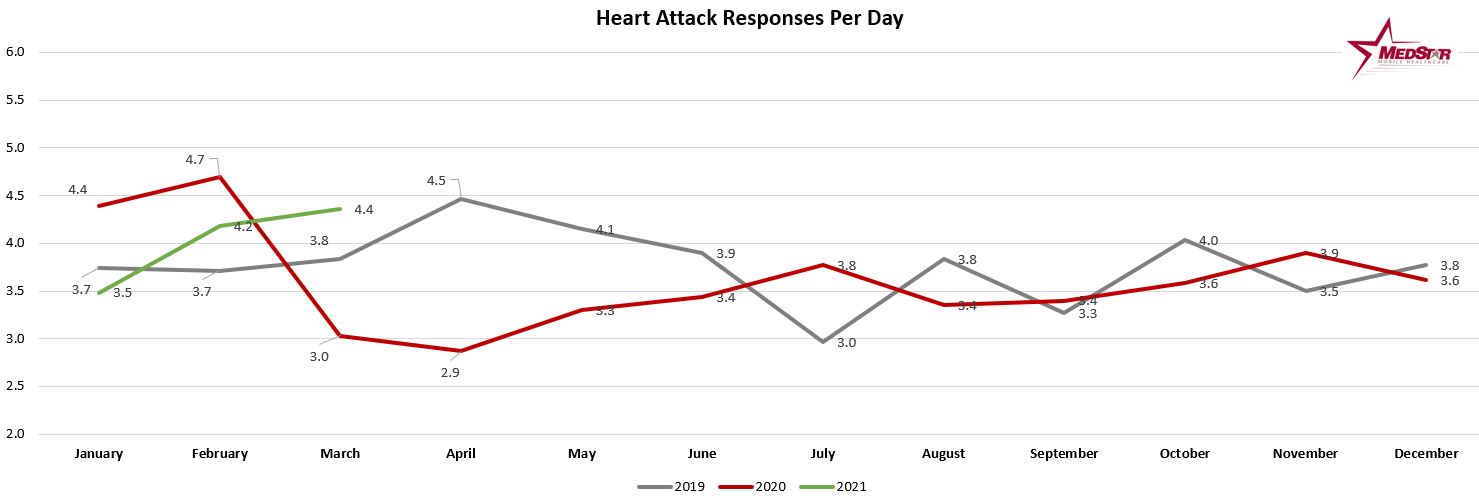
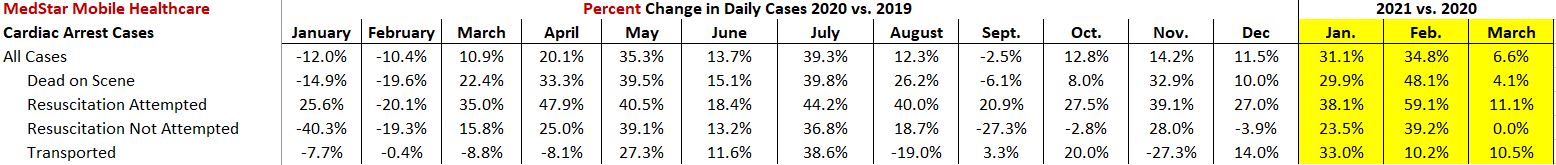
EMS providers and other healthcare experts continue to encourage people to not delay seeking medical care for potentially serious medical complaints.
Excerpts from the study and full study link:
—————–
Worse Cardiac Arrest Outcomes During The COVID-19 Pandemic In Boston Can Be Attributed To Patient Reluctance To Seek Care
Christopher Sun, Sophia Dyer, James Salvia, Laura Segal, and Retsef Levi
PUBLISHED: MAY 26, 2021
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2021.00250
Conclusion
The indirect effects of COVID-19 pose substantial immediate and long-term public health challenges. During the pandemic, patient avoidance and reluctance in seeking emergency care via EMS significantly increased compared with historical baselines. The avoidance of care and resulting possible treatment postponement likely played a critical role in the excess out-of-hospital cardiac arrests observed during the same time. The sustained changes in patients’ care-seeking behaviors and excess OHCA deaths after the initial COVID-19 wave may foreshadow the harmful long-term indirect effects of COVID-19 on health care systems. Ensuring that patients seek timely care during and after the pandemic is essential, to reduce potentially avoidable excess cardiovascular disease deaths.
Abstract
Delays in seeking emergency care stemming from patient reluctance may explain the rise in cases of out-of-hospital cardiac arrest and associated poor health outcomes during the COVID-19 pandemic.
In this study we used emergency medical services (EMS) call data from the Boston, Massachusetts, area to describe the association between patients’ reluctance to call EMS for cardiac-related care and both excess out-of-hospital cardiac arrest incidence and related outcomes during the pandemic. During the initial COVID-19 wave, cardiac-related EMS calls decreased (−27.2 percent), calls with hospital transportation refusal increased (+32.5 percent), and out-of-hospital cardiac arrest incidence increased (+35.5 percent) compared with historical baselines. After the initial wave, although cardiac-related calls remained lower (−17.2 percent), out-of-hospital cardiac arrest incidence remained elevated (+24.8 percent) despite fewer COVID-19 infections and relaxed public health advisories. Throughout Boston’s fourteen neighborhoods, out-of-hospital cardiac arrest incidence was significantly associated with decreased cardiac-related calls, but not with COVID-19 infection rates. These findings suggest that patients were reluctant to obtain emergency care. Efforts are needed to ensure that patients seek timely care both during and after the pandemic to reduce potentially avoidable excess cardiovascular disease deaths.
Change In Characteristics And Outcomes:
Beyond increased OHCA incidence, worse OHCA outcomes may also demonstrate the repercussions of patient reluctance and COVID-19. While assessing these relationships, OHCA patient and response characteristics with confounding effects on OHCA outcomes must also be examined. Accordingly, both the changes in OHCA outcomes and cofounding patient and response characteristics were assessed during and after the initial COVID-19 wave, relative to the historical baselines.
Discussion
This study supports the hypothesis that treatment delays resulting from increased patient reluctance to obtain urgent care contributed to the increased absolute and relative volume of non–nursing home out-of-hospital cardiac arrest incidence and death during the COVID-19 pandemic. Specifically, the substantial decrease in cardiac calls and increase in hospital transportation refusals during the pandemic supports the hypothesis of increased patient reluctance to seek EMS and in-hospital care.
As positive cardiac outcomes are dependent on timely treatment after symptom onset,12–14 these prolonged delays could explain the significantly increased rates of OHCA incidence and poor outcomes. In fact, these treatment delays may play a larger role in increasing OHCA incidence compared with the direct impact of COVID-19 infection.5,26
The Poisson regression analysis indicated that OHCA incidence was strongly associated with increased reluctance to call EMS and the initial COVID-19 wave period, during which barriers of obtaining care were abundant (for example, infection fears, financial instability, and stay-at-home advisories), but not with neighborhood-level COVID-19 infection rates.
Importantly, patients’ reluctance to seek emergency care and OHCA incidence remained elevated despite the low COVID-19 infection rates and relaxed public health advisories after the initial COVID-19 wave. This not only suggests the greater impact of patient reluctance on excess OHCA incidence compared with COVID-19 infections but also raises concerns regarding the potential long-term indirect effects of COVID-19. Lasting changes in patients’ care-seeking behaviors that worsen the underuse of EMS could result in increased mortality rates for acute conditions.9–12
The increased EMS avoidance and hospital transportation refusals during the pandemic were likely driven by patients’ reluctance to obtain care as opposed to unneeded medical attention. The decreased cardiac call volume and higher proportion of OHCAs among all cardiac calls suggests that at least some of the patients were only calling EMS during extreme emergencies. There is also evidence that some patients acted against explicit medical advice and refused transportation to a hospital after calling EMS. At least some of these patients experienced OHCA less than seven days after their initial EMS call, indicating that these refusals occurred despite worsening conditions. Moreover, historically, transportation refusals represent a reluctance to obtain necessary care, as approximately one in five patients refusing transportation received subsequent care at an emergency department within forty-eight hours after their refusal.27,28 Increases in refusal rates during the pandemic may similarly indicate higher patient reluctance to obtain care.