Special thanks to Harriet Ramos of the Fort Worth Star-Telegram for this excellent summary of the future EMS options analyzed in the Fitch report!
Residents of Fort Worth and the other member cities that are part of the EMS Authority should watch this issue very closely, as the Fort Worth City Council considers these options. Their decision will have significant clinical, operational, and fiscal implications for the future of EMS, and costs, in this region!
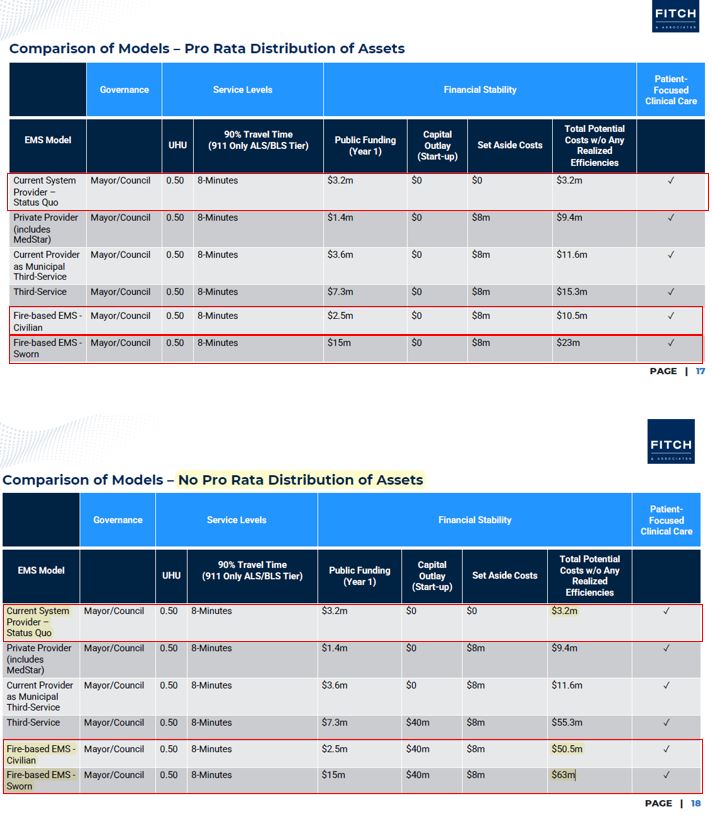
The basic consideration? Retain a world class EMS agency that is one of the most highly recognized and most economically efficient EMS system in the country for a public funding impact of $3.2 million, or ‘test’ a new model for somewhere between $15 million to $63 million, according to the Fitch analysis.
The next Fort Worth City Council Ad Hoc Committee on EMS is today at 12n and can be viewed live (or watched on demand after the meeting here: https://fortworthgov.granicus.com/player/camera/2
————————-
Assessment of Fort Worth’s EMS system nears end; 4 alternative models under consideration
BY HARRIET RAMOS
MARCH 18, 2024
https://www.star-telegram.com/news/local/fort-worth/article286426460.html
The independent consultant hired to assess Fort Worth’s EMS system is set to give its final report to the Ad Hoc Council Committee on Emergency Medical Response on Tuesday.
Over the next few weeks the committee will review the options provided by Fitch and Associates and give the Fort Worth City Council their recommendation on the best path forward for EMS service.
MedStar began servicing Fort Worth in 1986. The current service area includes Fort Worth and 13 surrounding cities, including Haltom City, White Settlement, Saginaw, Sansom Park and Westworth Village, according to the agency’s website.
MedStar received subsidies from Fort Worth and the other member cities until 2010. Expenses were low and the income generated from insurance payments and the Mobile Integrated Healthcare program made the ambulance service provider self-sustaining for several years.
According to Fitch’s report, MedStar will need public subsidies again due to rising costs and flat net revenues, something MedStar spokesperson Matt Zavadsky said the agency has been saying for some time.
“We’ve been very supportive of this process, and honestly Fitch has done a really good job with the study, with the data analytics,” Zavadsky said. “They have essentially validated everything that we’ve been saying for the last three years.”
CURRENT EMS PROVIDER
MedStar is “one of the least understood organizations in the community,” Zavadsky said. People tend to think of MedStar as a private company, but it’s actually a governmental administrative agency which is owned by the 14 member cities.
According to the agency’s website, teams from 220 communities across 46 states and six countries have visited MedStar over the past 10 years to learn about their EMS system. MedStar is also one of a handful of EMS agencies in the United States that is both certified and accredited to perform enhanced blood tests in the field to better pinpoint patients’ medical needs. Financial constraints have been a growing concern in recent years, Zavadsky said.
Costs have gone up and revenue from ambulance transports hasn’t kept pace. Medicare and Medicaid patients represent around 55-60% of MedStar’s cases, and there hasn’t been a Medicaid rate increase for ambulance service since 2007, according to Zavadsky.
Staffing shortages after COVID-19 have also played a factor as the cost of wages to retain emergency medical technicians and paramedics or attract new ones has skyrocketed, Zavadsky said.
In September, the Fort Worth City Council approved $4.2 million in transitional funding to cover MedStar budget shortfalls while the Ad Hoc Council Committee on Emergency Medical Response reevaluated MedStar’s services and reviewed other potential EMS models.
MedStar later decided the funding from the city wasn’t necessary. MedStar’s Chief Executive Officer Ken Simpson told the Star-Telegram in January that MedStar will be contracting with John Peter Smith Hospital to pay for inmate transports from the county jail. The city of Fort Worth will reimburse MedStar for inmate transports from the city jail. “Them taking responsibility for those patients and a couple other things we were able to do within the budget gave us the opportunity to balance the budget for this year while we work through this ad hoc process,” Simpson said.
The most recent Fitch and Associates report, presented to the ad hoc committee on Feb. 20, laid out four alternative EMS models for the committee’s consideration, including changing MedStar’s board but keeping “the current provider model without any additional substantive changes.”
ALTERNATIVE MODELS
The four EMS service delivery model options are each designed to provide high-quality patient care, according to Fitch’s report. They would all require public finding and would be governed by the Fort Worth Mayor and City Council.
They are also based on an eight-minute travel time, which doesn’t include the time required to answer the call and dispatch the ambulance.
The first model would retain MedStar in its current role but transfer governance to the Fort Worth City Council.
The second would replace MedStar with a fire-based EMS model operated by the Fort Worth Fire Department using either sworn or civilian personnel.
The third would establish a third public safety service in Fort Worth to handle emergency medical services.
The fourth would utilize a private contractor.
Keeping MedStar in its current role with a change of governance would cost an estimated $3.2 million. The entirety of that amount represents the cost for the first year of public funding.
This model maintains “the greatest degree of status quo,” according to the report. It would also be the easiest to implement since the only change would be to replace MedStar’s current 11-member board of directors with the Fort Worth City Council. MedStar’s current board consists of nine voting members along with the CEO and the EMS system medical director as non-voting members. Fort Worth appoints four of the voting members, and one of them is traditionally a member of the city council. The other three positions are usually held by a health care expert, an attorney and a community member, Zavadsky said. A fifth Fort Worth board position is always held by the city’s fire chief.
The 13 other member cities appoint one person to represent their communities, and the remaining members are appointed by the Emergency Physicians Advisory Board and the First Responder Advisory Board. According to Zavadsky, the variety of perspectives represented on the board is intentional and ensures the board remains non-political.
The estimated cost of adopting a fire-based EMS model would vary depending on the type of personnel used and whether or not the member cities agree to dissolve MedStar and distribute its assets. Fort Worth firefighters are trained EMTs and already respond to serious medical emergencies along with MedStar. If the fire-based model were adopted, the Fort Worth Fire Department’s role would expand to transporting patients to local hospitals. The total potential cost for the fire-based model is $63 million utilizing sworn firefighters and $50.5 million utilizing civilians if the city doesn’t receive any MedStar assets. If the city does receive MedStar assets, the projected cost drops to $23 million for sworn firefighters and $10.5 million for civilians. Dallas Fire-Rescue is an example of a fire-based EMS that uses sworn firefighters, and the Philadelphia Fire Department is an example of a civilian model.
The cost of creating a third Fort Worth public safety service to take over emergency medical services could cost $55.3 million if the city does not receive MedStar’s assets and $15.3 million if the city does. According to the report, this model would also require the longest time for implementation and transition since the city would essentially be creating this third service from scratch.
MedStar could potentially be used for this service, according to the report. The total projected cost utilizing MedStar would be $11.6 million. Austin-Travis County EMS is an example of this model.
The projected cost for implementing a private contractor model is $9.4 million. Under this model, the city of Fort Worth would contract with a private EMS provider for an agreed upon rate per hour. The city also would have the option of contracting with MedStar. The cost for this model would be less than the second and third options and the city could collect net revenues from ambulance transports, according to the report. The city of Arlington uses a private contractor for its EMS needs.
MEMBER CITIES
According to Zavadsky, Fort Worth represents 90% of MedStar’s call volume due to its population of nearly 1 million. The other 10% of the calls are spread throughout the other 13 member cities which range in size from around 46,000 people in Haltom City to less than 1,000 in Westover Hills. Westworth Village, a city of around 3,000 people and home of the Naval Air Station Joint Reserve Base, has been a MedStar member since the beginning, according to City Administrator Brandy Barrett.
Westworth Village and the other member cities, with the exception of Fort Worth, get together and vote for one person to represent them on MedStar’s board of directors.
Mayor Kelly Jones acknowledged that they don’t have any real power compared to Fort Worth’s five voting members, but at least they have “a seat at the table.”
It’s not clear how the other member cities would be affected if the Fort Worth City Council votes to replace MedStar’s current board of directors or do away with MedStar altogether.
Barrett told the Star-Telegram in a phone interview Friday that she’s attended meetings where Fitch presented reports of its findings, but the independent consultant hasn’t reached out to their city for input. “I don’t knock Fort Worth for doing their due diligence to make sure their citizens are best served,” Barrett said. “I just think that all of the areas should be considered, because they’re not the only ones being impacted by any potential change.”
Jones said the city leaders are trying to be proactive and learn as much about the alternative EMS models under consideration as possible.
“I want to keep an open mind when we visit with the Fitch group and with the Fort Worth council committee, you know. Unless they change our minds, we think the status quo is best, keeping MedStar as it is,” Jones told the Star-Telegram in a phone interview Friday.
From his perspective, “keeping MedStar as is” also means keeping MedStar’s board of directors in place, according to Jones.
Barrett said Westworth Village is willing to help subsidize MedStar if the Fort Worth City Council votes to keep the current EMS provider, but the city want to make sure it has proper representation when the amount is determined.
“We want to make sure that the share is fair and we have some control, or at least some input, on how that is calculated in the future,” she said. Westworth Village uses its police officers as medical first responders in the same way that Fort Worth uses firefighters.
When the city had to do away with its volunteer fire department and contract with Fort Worth for fire service, Westworth Village found it was cheaper to use Fort Worth for fire only and use its own police to respond to medical emergencies, Jones said. The officers stabilize the patients at the scene and advise MedStar about their condition so MedStar can take immediate action when the ambulance arrives, according to Jones. He estimates the city has saved around $300,000 a year by using its police force as first responders instead of contracting that service out.
According to Barrett, MedStar trained the city’s police officers. They also communicate regularly with the other member cities and keep them informed of what is going on. “When we do have … a call that doesn’t seem to go the way we think it should, they’re very responsive when we call and ask about it,” Barrett said.
Jones has invited the mayors and administrators of the member cities, with the exception of Fort Worth, to a meeting to make sure they are all aware of what Fort Worth is considering with EMS services and get their thoughts on it.
“From my perspective, we’re very pleased (with MedStar’s services),” Jones said. “They do a good job. They get here timely, they’re professionals, their staffs are professional, so we’re pleased with the status quo and we hope it continues.”
—————————–
To see facts about MedStar “one of the least understood organizations in the community,”, click here: https://www.medstar911.org/category/news-and-press-releases/
To learn more about MedStar, and the EMS system, feel free to visit the Fort Worth City Manager’s EMS FAQs here: https://www.fortworthtexas.gov/departments/citymanager/med-star
To learn more about the ongoing EMS System assessment, click the City of Fort Worth news release here: https://www.fortworthtexas.gov/news/2024/2/ems-fitch-recommendations
And, a recent news from the Fort Worth Report here: https://fortworthreport.org/2024/02/20/fort-worth-is-considering-four-potential-ems-models-heres-what-theyd-do/






